ISSN 2764-1449 | ISSN (Online) 2764-1430


Ane Caroline Gaspardi1; Francisco Guilherme Fujita Neto2
Abstract
INTRODUCTION: According to Article 6 of Consolidation Ordinance No. 5 of November 22, 2017 (Origin: PRT MS/GM 158/2016), “the transfusion of blood and its components shall be used judiciously in medicine, since every transfusion carries in itself a risk to the recipient, whether immediate or delayed, and must be indicated judiciously.” Therefore, the objective of this study was to verify the general profile of transfusion requests, as well as the hemocomponents prescribed, evaluating mainly patients treated with red blood cells on an emergency basis.
METHODS: A search was conducted in the FUJISAN computerized system for Transfusion Requests (TR) recorded from July 1, 2020 to July 31, 2021. The results were tabulated in Excel spreadsheet for analysis.
RESULTS: A total of 21,768 transfusion requests were registered in the period, resulting in the prescription of 58,218 blood products to 13,823 patients. Of these, only 300 were performed on an emergency basis.
CONCLUSION: It is concluded that although emergency requests are the minority, the concern with alloimmunized patients remains, in addition to the under-reporting of transfusion reactions, suggesting the need for improvements in the communication system with hospitals to highlight the importance of hemovigilance.
INTRODUCTION
According to Article 6 of Consolidation Ordinance No. 5 of November 22, 2017 (Origin: PRT MS/GM 158/2016), “the transfusion of blood and its components shall be used judiciously in medicine, since every transfusion carries in itself a risk to the recipient, whether immediate or delayed, and must be indicated judiciously.” According to current legislation, there are four types of transfusion, namely: scheduled, routine, urgent and emergency1. When the delay in transfusion could be life-threatening (emergency), the special transfusion protocol is activated and group “O” Negative red cell concentrates can be used without completing the pre-transfusion tests, as long as clinically justifiable , with the prescribing physician being responsible for such an act2.
Although it is allowed, pre-transfusion testing is essential to ensure transfusion safety, especially for patients alloimmunized against red blood cell antigens other than the ABO system and RhD antigen, such as Rh, Kell, Kidd, Duffy, MNS, Diego, among others. In emergency situations, when tests are not performed prior to transfusion, and therefore possible clinically significant alloantibodies are not identified in a timely manner, the recipient runs the risk of severe, potentially fatal hemolytic reactions3. Therefore, the objective of this study was to verify the general profile of transfusion requests, as well as the hemocomponents prescribed, evaluating mainly patients that received red blood cells on an emergency basis.
METHODS
The computerized system of FUJISAN - Centro de Hemoterapia, Hematologia e Terapia Celular do Ceará LTDA. was searched for transfusion requests (TR) recorded in the period from July 1, 2020 to July 31, 2021. The information extracted was tabulated in Excel spreadsheet, consisting of the transfusion modality (1 - scheduled, 2 - routine, 3 - urgent, 4 - emergency and 5 - reserve), type and amount of blood products prescribed (RBC - Red blood cell, PC - platelet concentrate, APC - apheresis platelet concentrate, PFC - fresh frozen plasma, CRIO - cryoprecipitate, and CP - convalescent plasma). The incidence of transfusion reactions and history of alloimmunization against red blood cell antigens of the patients seen during this period were also evaluated.
Among the transfusion modalities, we evaluated the profile of patients admitted with RC in an emergency basis, based on the following variables: gender, age, diagnosis and clinical protocol. Data were collected only after the consent of the medical director.
RESULTS
A total of 21,768 transfusion requests were registered in the established period, which resulted in the prescription of 58,218 blood components for 13,823 patients. Among the requests, 1,476 (6.8%) were programmed, 8,285 (38.1%) routine, 4,147 (19.1%) urgent, 300 (1.4%) emergency and 7,560 (34.6%) reservations. The amount of blood components prescribed in each modality is shown in table 1.
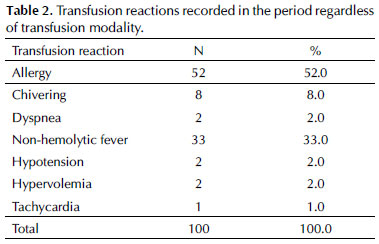
Despite the high number of requests and blood components prescribed, only 100 transfusion reactions were recorded, which alerts us to possible under-reporting. The most prevalent was the allergic reaction, with 52% of the cases, 34% mild, 14% moderate, and 4% severe. The other reactions are shown in table 2.
With regard to the incidence of alloimmunization, about 5% of our 13,823 patients have irregular antibodies against the major blood group systems, with 70% of cases directed toward antigens of the Rh and Kell systems. Among the alloimmunized patients, 447 have clinically significant antibodies at undetectable levels on pretransfusion testing.
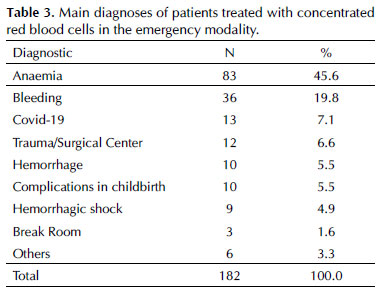
Although the rate of transfusions performed in the emergency setting corresponds to only 1.4% of the evaluated requests, we verified the profile of patients linked to 182 requests that prescribed 368 concentrated red blood cells. A total of 94 male patients, 82 female patients, and 06 newborns were analyzed. The median age was 54 years (0 to 98 years), with no statistical difference between genders. The main diagnoses and clinical protocols are shown in tables 3 and 4, respectively.
DISCUSSION
The numbers of transfusion requests per modality are consistent with each analyzed category. We observed that although the reservations comprise 34.6% of the requests, operationally, the level of this type of request with patients already in the operating room, undergoing previously scheduled procedures, is quite high. This conduct may result in the emergency release of blood components, exposing the patient to risks potentially controlled if the reserve was made in a timely manner as recommended by the legislation in force.
The availability of a safe blood supply is a critical component of transfusion medicine. Stocks of group “O” Negative RBCs and group “AB” plasma are of prime value in a blood bank4. However, according to the bulletin issued by the AABB, there are three criteria for the appropriate use of these RBCs: mandatory, for patients sensitized with anti-D and women of childbearing age; recommended, for bone marrow transplant candidates, those with aplastic anemia or cancer; and acceptable release of “O” Positive, in the case of patients over 45. In addition, it is fundamental to transfuse only the necessary units, mainly because it is a scarce resource2.
Transfusion is a therapy with widespread benefits, but with intrinsic risks leading to increased morbidity and mortality5. The application of measures to detect the need for transfusions in the Emergency Department or even to activate massive transfusion protocols can help in the rational use of blood6. According to Alimohammadi, 20177 the evaluation of parameters such as hypotension, presence of free fluid on ultrasound, clinical instability of the pelvic ring, age, admission and mechanism of trauma, enabled only 6% of 793 patients to be transfused in the emergency.
Although the sensitization rate is relatively low, there are still potentially fatal risks, especially in emergency transfusions performed without the completion of pretransfusion testing. Alloimmunization causes several problems, from delay in obtaining compatible blood to hemolytic transfusion reactions8. The correct identification of these antibodies is fundamental to provide satisfactory transfusion support and requires highly specialized immunohematology teams, especially when dealing with rare antibodies9.
According to the guidelines recommended by PBM - Patient Blood Management, optimizing the patient’s blood preoperatively by increasing hemoglobin/hematocrit levels, and proposing alternatives such as intraoperative blood recovery and hemodilution, in addition to minimizing hemostatic disorders, improve clinical outcomes by avoiding unnecessary exposure to blood components. Strategies of this kind should be discussed and planned in advance8,10-11.
As cited earlier, about 3.2% of our patients had clinically significant alloantibodies undetectable on pretransfusion testing. According to Chonat, 201912, 30% of hemolytic transfusion reactions can occur under these conditions. A relevant point observed in our results was the small number of transfusion reactions reported, which denotes the occurrence of underreporting and suggests the need for improvements in the communication system with hospitals to highlight the importance of hemovigilance.
Another characteristic of our population was the age of the patients. Although the median age was 54 years, 34% of patients seen in the emergency modality were over 65 years old, and anemia was the most common finding among the requests. According to Loftus, 201813, anemia is common and morbid among the elderly, causing them to have lower hemoglobin levels compared to younger patients, despite receiving more transfusions. These data may reflect the impact of nutritional deficiencies, multiple medications, and myelodysplasia in this population. Because they respond less to transfusion, exogenous administration of iron and erythropoietin may have therapeutic value in this group of patients.
CONCLUSION
Although the transfusion requests made in the emergency mode characterize the minority of cases, there is still a concern about alloimmunized patients and about the management of group “O” Negative RBC concentrate to maintain an adequate stock. Moreover, the high number of requests and blood products prescribed, compared to the record of only 100 transfusion reactions, alerts us to possible underreporting, suggesting improvements in the communication system with hospitals to highlight the importance of hemovigilance.
REFERENCES
1. Brasil. Portaria de Consolidação no 5 de 28 de setembro de 2017. Consolidação das normas sobre as ações e os serviços de saúde do Sistema Único de Saúde. Ministério da Saúde [Internet]. 2017;926. Available from: http://portalarquivos2.saude.gov.br/images/pdf/2018/marco/29/PRC-5-Portaria-de-Consolida----o-n---5--de-28-de-setembro-de-2017.pdf
2. Murphy M BD. Recommendations on the Use of Group O Red Blood Cells. AABB Assoc Bull 19-02 2019. 2019;(D):1–12.
3. Pirenne F. Prevention of delayed hemolytic transfusion reaction. Transfus Clin Biol [Internet]. 2019;26(2):99–101. Available from: https://doi.org/10.1016/j.tracli.2019.02.007
4. Gammon RR, Rosenbaum L, Cooke R, Friedman M, Rockwood L, Nichols T, et al. Maintaining adequate donations and a sustainable blood supply: Lessons learned. Transfusion. 2021;61(1):294–302.
5. Medvecz A, Bernard A, Hamilton C, Schuster KM, Guillamondegui O, Davenport D. Transfusion rates in emergency general surgery: High but modifiable. Trauma Surg Acute Care Open. 2020;5(1):1–5.
6. Horst K, Lentzen R, Tonglet M, Mert Ü, Lichte P, Weber CD, et al. Validation of the mTICCS Score as a Useful Tool for the Early Prediction of a Massive Transfusion in Patients with a Traumatic Hemorrhage. J Clin Med. 2020;9(4):945.
7. Alimohammadi H, Kianian Y, Zerepoosh F, Derakhshanfar H, Alavi-Moghadam M, Hatamabadi H, et al. Accuracy of emergency transfusion score in prediction need for blood transfusion among multiple trauma patients: A cross-sectional study from Iran. Int J Crit Illn Inj Sci. 2017;7(4):248–51.
8. Deepti Sachan; Aseem K. Tiwari; Ravi Dara; Dinesh Jothimani; Ilankumaran Kaliamoorthy; Srinivas Mettu Reddy; Mohamed Rela. Patient blood management in a patient with multiple red cell antibodies (anti-C, anti-e, and anti-K) undergoing liver transplant in South India: A team approach. Asian J Transfus Sci. 2020;14((1)):74–8.
9. Santos LD, Bub CB, Aravechia MG, Bastos EP, Kutner JM, Castilho L. The rare holley antibody associated with a severe hemolytic transfusion reaction: the importance of this antibody identification to find a compatible blood unit. Einstein (São Paulo). 2020;18:eRC4582.
10. National Blood Authority. Critical Bleeding Massive Transfusion : Module 1. Patient Blood Manag Guidel [Internet]. 2011;1–112. Available from: https://www.blood.gov.au/pbm-guidelines
11. Meybohm P, Straub N, Füllenbach C, Judd L, Kleinerüschkamp A, Taeuber I, et al. Health economics of Patient Blood Management: a cost-benefit analysis based on a meta-analysis. Vox Sang. 2020;115(2):182–8.
12. Chonat S, Arthur CM, Zerra PE, Maier CL, Jajosky RP, Yee MEM, et al. Challenges in preventing and treating hemolytic complications associated with red blood cell transfusion. Transfus Clin Biol [Internet]. 2019;26(2):130–4. Available from: https://doi.org/10.1016/j.tracli.2019.03.002
13. Loftus, Tyler J.; Brakenridge, Scott C.; Murphy, Travis W.; Nguyen, Linda L. Moore, Frederick A.; Efron, Philip A; Mohr AM. Anemia and blood transfusion in elderly trauma patients. J Surg Res. 2018;229:288–93.